Different faces, shared targets: the curious convergence of AD, AA, and vitiligo
In the evolving landscape of dermatology and clinical immunology, a compelling paradox is emerging: three phenotypically distinct conditions—atopic dermatitis (AD), alopecia areata (AA), and vitiligo—are increasingly found to share overlapping immunological features and respond to similar targeted therapies.
Historically, the connections among these disorders were considered tenuous at best. While AA has long been loosely associated with atopy, its relationship with AD was more correlative than causative. Vitiligo, until only two decades ago, was not widely recognized as related to the atopic diathesis. Today, however, advances in genetics and immunopathology are reframing these diseases not as isolated entities, but as members of a broader immunological spectrum—challenging the notion that distinct clinical presentations necessarily reflect unrelated pathogenic mechanisms. A similar reevaluation is now being applied to the traditional dichotomy between AD and psoriasis, especially in light of recent insights from immunomodulatory treatments.
AD, for example, is hallmarked by intense pruritus and eczematous inflammation; AA by sudden, non-scarring hair loss; and vitiligo by melanocyte loss causing progressive depigmentation—each affecting different target structures and exhibiting unique symptom profiles. Despite these differences, patients with one condition may present with or develop another, and targeted or semi targeted immunotherapies such anti TH2 biologics or JAK inhibitors have demonstrated efficacy across all three. Paradoxically, these treatments have also been implicated in inducing phenotypes resembling AD, AA, or vitiligo in some patients. This convergence raises important questions about whether the observed effects stem from off-target actions or reflect broader immunological circuit modulation that is not yet fully understood. Within this framework, seemingly naive questions—such as “Why is pruritus typically absent in vitiligo or AA?”—can prompt us to reconsider fundamental aspects of disease biology that may have been overlooked due to a historically compartmentalized, clinicopathologic approach to dermatologic classification.
Mechanistic insights summarized in a recent Journal of Allergy and Clinical Immunology review (DOI: 10.1016/j.jaci.2025.04.016) highlight the involvement of tissue-resident memory (TRM) cells, IFN-γ signaling, and a network of shared cytokines—particularly IL-15, IL-9, and IL-21—across AD, AA, and vitiligo (DOI: 10.1016/j.jaci.2025.04.016). These immune pathways contribute to disease chronicity, tissue-specific autoimmunity, and relapse. Importantly, their modulation can alter disease expression even in tissues not overtly involved in the primary pathology. This rather paradoxical therapeutic overlap likely reflects systemic immune circuit engagement rather than the correction of any single pathogenic trigger. Furthermore, shared genetic susceptibility loci support the concept of a common immunological foundation across these clinically distinct entities.
As our understanding of the skin’s immune and nervous systems deepens, the boundaries between these diseases may become more functionally defined rather than strictly categorical. These insights do not necessitate the abandonment of established disease classifications, but they do advocate for a more nuanced framework. Ongoing research into these converging pathways with diverging clinical features holds the potential to inform more precise, mechanism-based therapeutic strategies for these interconnected inflammatory skin disorders.
RAJKA-ISAD 2025:
The Call for Abstract is open!

GET READY!
- Submit your abstract before July 15th (notification of acceptance in late August)
- Registration system starts on June 5th!
- Meeting from October 24 to 26, 2025
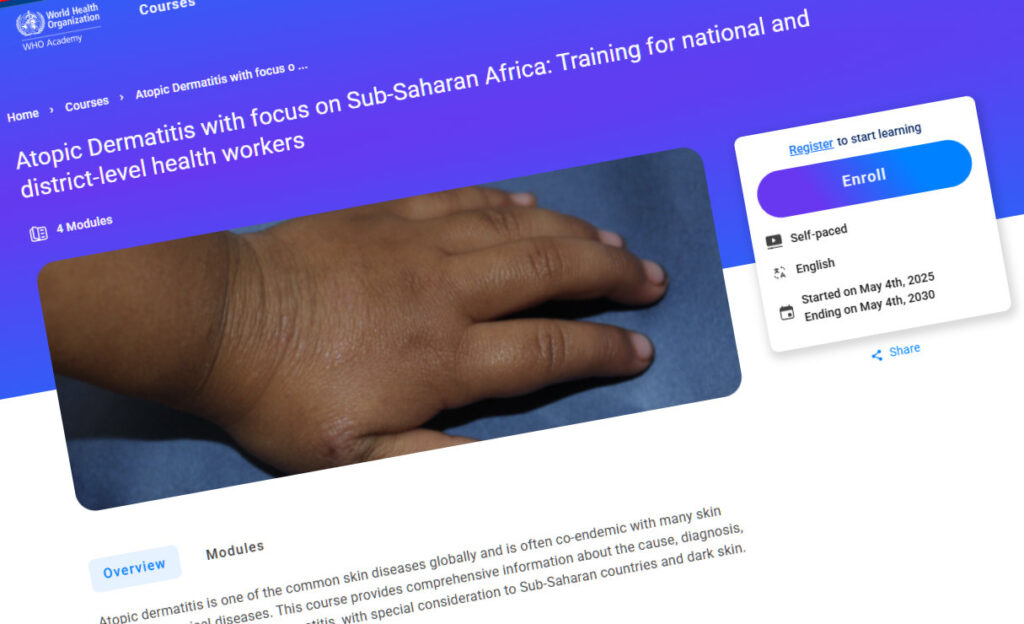
ISAD-WHO course again published on the WHO academy platform
Research & Fellowships

ISAD × GADA fellowship results
A heartfelt thank you to everyone who applied. We were genuinely encouraged by the volume and quality of submissions we received.
We are delighted to inform that Dr Gloria MASENGA from Tanzania has been selected for the ISAD-
GADA Fellowship with her project “Epidemiology of Atopic Dermatitis in an African Population Living in the Kilimanjaro Region, Northeastern Tanzania.” —congratulations! We look forward to sharing updates on her important research.
ISAD RESEARCH FELLOWSHIP
- Advance your research career with the prestigious ISAD Research Fellowship – apply today!
Don’t miss this opportunity to contribute to cutting-edge dermatology research. Learn more about the ISAD Research Fellowship! [link]
MORE FROM GADA
- Are you interested in Harmonising epidemiology study designs for AD Research?
You are invited to share your views and take part in a consensus exercice: [link]
#StayInformed:
Explore the Latest in AD Research!
News on PubMed:
Dive into our curated selection of cutting-edge studies from PubMed, offering valuable insights into various aspects of Atopic Dermatitis:
- AD hidden hematologic risk: clonal hematopoiesis of indeterminate potential (CHIP)
- An unusual facial bump related to AD
- Switching off selectively skin lipid synthesis: a reversible human model of ceramide depletion
- Beyond the skin: suicidal risk is real in AD
- Complement, an overlooked driver of Th2 Immunity in AD


